Fragile X syndrome (FXS), also known as Martin-Bell syndrome or marker X syndrome, is an inherited genetic illness that causes, among other problems, developmental delays, intellectual disabilities, and/or autistic spectrum disorder. It is the most prevalent genetic form of intellectual and developmental disability (IDD) after down syndrome (Trisomy 21). [1] FXS is referred to as fragile X syndrome because, under a microscope, a segment of the X chromosome appears “broken” or “fragile.” [2]
Herbert A. Lubs, an American genetics educator, was the first to identify an atypical “marker X chromosome” linked to intellectual impairment in 1969. And then, in 1970, Frederick Hecht introduced the phrase “fragile site”. Finally in 1985, Felix F. de la Cruz elaborated on the physical and cytogenetic aspects of persons affected by the illness, as well as treatment prospects. [3]
FXS is one of three syndromes in the fragile X family. The other two syndromes are:
- Fragile X-associated tremor/ataxia syndrome (FXTAS): Balance issues, shaky hands, unstable mood, memory loss, cognitive issues, and numbness in the hands and feet are all symptoms.
- Fragile X-associated primary ovarian insufficiency (FXPOI): Reduced fertility, infertility, irregular or absent menstrual periods, and premature menopause are all symptoms. [2]
It is unknown how many people are affected by FXS, however a review of research studies estimates that approximately 1 in 7,000 males are affected. It’s less common in girls, about 1 in 11,000 females have been diagnosed with FXS. Typically, boys are diagnosed between the ages of 35 and 37 months, and girls at 42 months. You may begin to observe signs in your child as early as 12 months {4]. Generally speaking, boys have more severe symptoms than girls, although these symptoms are not life-threatening.
There are different signs a child might have FXS:
A child many have Intelligence issues:
- Learning disabilities.
- Low intelligence quotient (IQ). Their IQ scores decrease with age.
- Late to reach early milestones of development. (not sitting, walking, or talking with other kids the same age at the same time).
- Late development of nonverbal communication (using gestures, body language and facial expressions).
- Stuttering
Mental health issues:
- Anxiety.
- Depression.
- Obsessive compulsive behaviours.
Behavioural issues:
- Attention-deficit/hyperactivity disorder (ADHD).
- Social anxiety, shyness.
- Flapping or biting their hands.
- Poor eye contact.
- Difficulty picking up “social cues.”
Other health issues:
- Seizures (epilepsy).
- Difficulty sleeping
- obesity
Children with FXS have certain prominent physical features [5]:
- Long, narrow face.
- A large forehead and jaw.
- Soft skin.
- Large ears and crossed/lazy eyes.
- Very flexible or double-jointed fingers.
- Flat feet.
- A high-arched palate (the roof of the mouth).
- Low muscle tone.
There are thousands of genes in each cell of the human body. Genes determine many things about a person – such as; what the person will look like and if he or she is likely to get certain diseases. The instructions for making proteins in the cells are also in the genes. For the body to work right, it needs proteins.
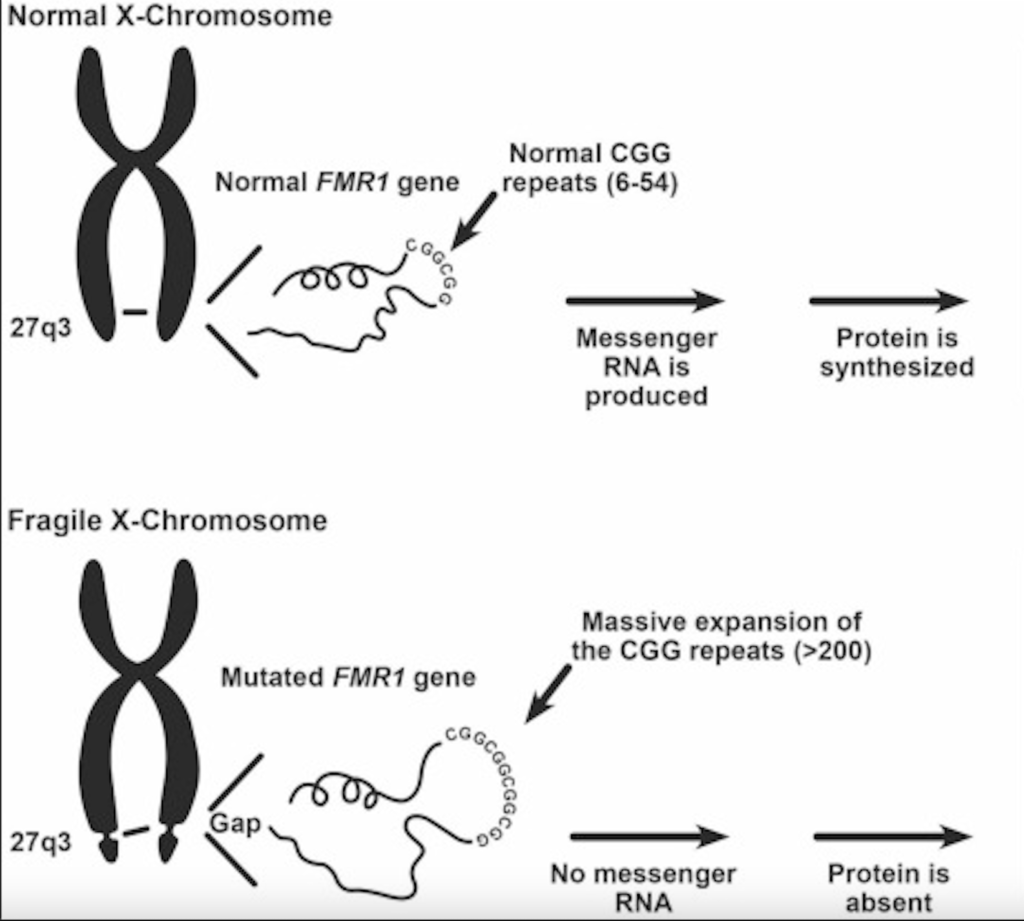
A change in the Fragile X Messenger Ribonucleoprotein 1 (FMR1) gene is what causes FXS. A protein called FMRP is made by the FMR1 gene. This protein is important for brain development and is not made by people with FXS. People with a mutated FMR1 gene don’t always have FXS symptoms. Some people can still make the FMRP protein because; they are female, the mutation is small, or only some of their cells changed (mosaicism).[2]
There is a spot in the FMR1 gene where the chemical letters CGG are repeated over and over again in a pattern. The CGG part of the DNA develops when the FMR1 gene changes. A normal part repeats five to forty times, but it repeats more than 200 times in people with fragile X syndrome.[4]
This repetition stops the FMR1 gene from making FMRP by “turning it off”. The FMR1 gene makes a protein called FMRP. Its main job is to selectively bind to about 4% of mRNA in the brains of mammals and move it out of the cell nucleus and to the synapses of neurons. Most of these mRNA targets have been found in the dendrites of neurons. Brain tissue from humans with FXS show abnormal dendritic spines, which are needed to make more connections between neurons. Because of this, there are problems with the formation and function of synapses and the growth of neural circuits. This affects neuroplasticity, which is an important part of learning and remembering.
Lack of FMRP slows down the production of mRNA and, in turn, protein synthesis, making LTD (Long Term Depression) worse. FMRP also seems to affect dopamine pathways in the prefrontal cortex. This is thought to be why people with FXS have trouble paying attention, being hyperactive, and controlling their impulses. The anxiety symptoms that are common in FXS may be caused by the down regulation of GABA (neurotransmitter that blocks impulses between nerve cells in the brain) pathways, which serve as inhibitors and help with learning and memory.[6]
The fragile X mutation is classified into four types by the number of times the CGG repeats in the DNA determines them. A blood test can be used to determine them:
- Normal: Most males have between 5 and 44 repeats of the chemical letters CGG in their FMR1 gene, and most females have between 5 and 44 repeats in each of their FMR1 genes. This is considered a reasonable number of repetitions. People who have a normal number of repeats do not have FXS and do not pass a higher risk to their children.
- Gray zone: People with an intermediate number of repeats (45 to 54) do not have FXS and are not at risk of having FXS children. They may, however, have a slightly increased risk of having some symptoms associated with other fragile X-associated disorders and may pass this risk on to their children.
- Premutation carrier: People with 55 to 200 repeats in the FMR1 gene are said to have a “premutation” in the gene. They do not have FXS, but they may have or develop other fragile X-associated disorders in the future. Furthermore, people who have a premutation can have children who have a premutation or a full mutation (FXS). However, the chances of having a child with a premutation or a full mutation differ between men and women who have a premutation.
A woman with a premutation can pass on a full mutation to her offspring. The greater the number of CGG repeats a woman with a premutation has, the more likely her child will inherit a FMR1 gene with a full mutation and, as a result, have FXS. A woman who has a premutation in one of her FMR1 genes has a 50% chance of passing on the premutation or a full mutation to her child.
A man who has a premutation will pass it on to his daughters but not to his sons. A father who has a premutation will not pass on a full mutation to his children.
- Full mutation: People with FXS have a full mutation (more than 200 repeats). Women have a 50% chance of passing fragile X to their child with each pregnancy (sons or daughters).
It’s important to remember that the FMR1 gene is on the X chromosome. A female has two copies of the FMR1 gene, one on each of her two X chromosomes [6]. Because of this, each copy of the FMR1 gene usually has a different number of CGG repeats. For example, a female’s FMR1 gene could have 30 CGG repeats on one copy and 70 CGG repeats on the other copy. The number of CGG repeats in a female’s FMR1 gene copy determines which group she is in (normal, intermediate, premutation, or full mutation, as shown below). Males only have one X chromosome, so they only have one copy of the FMR1 gene. The number of CGG repeats in that one copy determines which group a male is in.
Fragile X syndrome must be diagnosed using DNA from blood, amniotic fluid, or other tissues. Various prenatal tests (amniocentesis, chorionic villus sampling) [2] can be used to determine whether a child has Fragile X Syndrome.
FXS has no known cure. Treatment services, on the other hand, can assist people in learning important skills. Therapy to learn to talk, walk, and interact with others is one example of a service. Furthermore, medicine can be used to help control some issues, such as behavioural issues. People with FXS, parents, and health care providers should collaborate closely to develop the best treatment plan, as should everyone involved in treatment and support—this may include teachers, childcare providers, coaches, therapists, and other family members. It is important to note that treatment plans should be individualized based on the person’s specific needs and abilities. Additionally, early intervention and consistent treatment can improve outcomes for individuals with FXS.
Reference:
- Medscape.com. (2019). Fragile X Syndrome: Practice Essentials, Background, Pathophysiology. [online] Available at: https://emedicine.medscape.com/article/943776-overview [Accessed 9 Mar. 2023].
- Cleveland Clinic. (n.d.). Fragile X Syndrome: Diagnosis, Symptoms & Treatment. [online] Available at: https://my.clevelandclinic.org/health/diseases/5476-fragile-x-syndrome#:~:text=It [Accessed 9 Mar. 2023].
- Wikipedia Contributors (2019). Fragile X syndrome. [online] Wikipedia. Available at: https://en.wikipedia.org/wiki/Fragile_X_syndrome [Accessed 9 Mar. 2023].
- CDC (2018). How Fragile X Syndrome is Inherited. [online] Centers for Disease Control and Prevention. Available at: https://www.cdc.gov/ncbddd/fxs/inherited.html [Accessed 9 Mar. 2023].
- Healthline. (2018). Fragile X Syndrome: Causes, Symptoms, and Diagnosis. [online] Available at: https://www.healthline.com/health/fragile-x-syndrome#symptoms [Accessed 9 Mar. 2023].
- Sidorov, M.S., Auerbach, B.D. and Bear, M.F. (2013). Fragile X mental retardation protein and synaptic plasticity. Molecular Brain, [online] 6(1), p.15. doi:https://doi.org/10.1186/1756-6606-6-15.